

Injury Prevention
Back Pain
Dr. Larry W. McDaniel, Ed.D., Carmyn Streitz, Allen Jackson, MS, and Laura Gaudet, Ph.D., discuss artificial disc replacement surgery, preoperative preparation, the surgical procedure, and postoperative recovery.
Back pain is a common health problem that affects most people at some point in their lives. Most back pain is not severe and may result from poor posture, improper body mechanics, or overexertion. About 50% of people older than 40 years of age have Degenerative Disc Disease (DDD), which is similar to osteoarthritis. Many people do not have pain, but for others, chronic pain can become a life-altering condition that affects their daily living and quality of life. Arthrodesis (i.e., spinal fusion) has been the treatment of choice for people with DDD, but this paper will discuss artificial disc replacement instead of spinal fusion.
The spine is a biomechanical phenomenon that allows flexion, extension, and a wide range of motion for the body. It naturally curves at the cervical, thoracic, and lumbar regions. The adult spine has four normal curvatures, from superior to inferior. Most injuries occur at the lower lumbar level because most of the torso's axial weight is distributed toward the pelvis. The vertebral body becomes more prominent toward the sacrum, carrying more weight.
Between each vertebra (Figure 1 - Vertebra (Bajnoczy 2009)[6]) is an intervertebral disc. Intervertebral discs (IVD) are fibrocartilaginous elastic cushions (i.e., shock absorbers) located between each vertebral body. These structures have high water content and a glycoprotein component called the nucleus pulposus. The intervertebral disc provides the intervertebral space height and stability. Most people are taller in the morning than in the evening because of the discs' water content compression throughout the day. |
Figure 1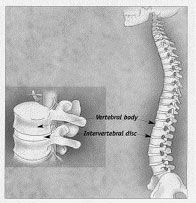 |
The annulus fibrosus outer ring of collagen fibres, surrounds the intervertebral disc. Tears in the annulus and subsequent ligament stretching can cause significant back pain because these structures have many nerve endings. Nerve roots in the spinal cord carry sensory messages from the brain and end in a bundle at the base of the spine called the cauda equina.
Degenerative disc disease occurs when an IVD becomes worn out because of ageing, damage, or trauma. The disc does not correctly cushion the vertebrae with DDD and distribute body weight. Discs can wear out, tear, bulge outward, or rupture through the annulus, causing pressure on the nerve and resulting in nerve impingement, inflammation, and pain. Nerve impingement can cause numbness and muscle weakness of extremities, sciatica, and even bowel or bladder problems. If this is left untreated, permanent nerve damage may occur. As discs wear down, bone spurs and osteophytes form on the vertebrae in a condition similar to osteoarthritis.
Patients are given a conservative course of treatment to ease pain and inflammation of their backs: Brief rest until the pain has decreased, moist heat to the affected area, muscle relaxant medications to treat pain-related muscle spasms, non-steroidal anti-inflammatory drugs, or steroid medications to relieve inflammation and pain, opioid analgesia for immediate relief, physical therapy and exercise to ease pain, improve mobility and flexion, and strengthen abdominal and back muscles to support the spine, and weight loss to decrease pain resulting from increased load-bearing.
Patients with Degenerative Disc Disease (DDD) (Figure 2 - Irvine Health, 2006) currently use spinal fusion to treat DDD. The diseased disc is removed in spinal fusion, and an autologous bone (iliac bone crest harvest or donor autograft) is placed in the space to create a bony fusion between the vertebrae. Sometimes, screws, rods, or interbody cages are implanted to stabilise the spine. Many patients experience pain relief after undergoing a spinal fusion. It is commonly theorised that the source of DDD pain is the movement of the involved segment and overall axial force instability. Spinal Fusion isolates and immobilizes the spine's painful motion segment and halts the degenerative process at that level. Not only does spinal fusion relieve pain, but it also provides spinal stability, re-establishes disc height, and slows down the degenerative process of the diseased disc. |
Figure 2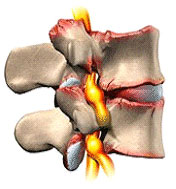 |
Approximately 200,000 people undergo discectomies with or without spinal fusion, with an overall success rate of 90%. Technological and osteological advances have made fusions more successful than ever and have made iliac bone crest harvest an option rather than a necessary choice. Doctors use titanium rods, screws, and interbody cages to help stabilize the vertebral bodies until fusion occurs. (Figure 3 - Medtronic, 2007) An advantage of titanium over stainless steel is that fluoroscopic images are not blurred, and allow for correct placement. Titanium is compatible with magnetic resonance imaging (MRI) scanning for future patient diagnostic testing. |
Figure 3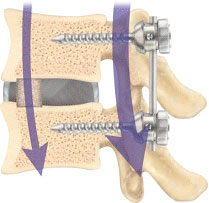 |
It takes approximately three to six months and can take as long as 18 months after bone graft and implants are surgically placed in the spinal segment to fuse. Physicians may recommend that the patient wear a brace or corset to support the back and encourage good posture. Physical therapy and exercise programs help the patient regain movement. Many patients experience relief of symptoms as pressure is taken off the irritated nerve roots. Some patients experience adverse effects, such as vascular or dural tears, chronic pain or stiffness, or failed back syndrome. Some of these ailments may require additional surgery.
Spinal fusion is not the only operation of DDD. In 2004, the FDA approved an artificial disc (Figure 4 - Rush University, 2008) to treat DDD. The artificial disc offers an alternative to spinal fusion to treat degenerative disc disease at these levels. It is designed to preserve spinal motion and recreate the natural function of the disc. There are specific criteria for artificial disc candidates. Patients must be between 18 and 60, have one diseased disc level at L4-5 or L5-S1, have DDD confirmed by medical history (MRI, x-ray, discogram, etc.), and have undergone six months of conservative treatment without experiencing relief of their back pain. |
Figure 4 |
The metal endplates of the implant must be able to grab onto the solid bone for the prosthesis to be effective, and the surgical approach is through the abdomen. Some contradictions to the surgery could be allergies to metal, autoimmune disorders, facet joint disease, history of chronic steroid use, infection, morbid obesity, osteoporosis, pregnancy, previous back surgery, spondylolisthesis greater than 3 mm, scoliosis, or a spinal tumour. Some postoperative complications involving abdominal and spine surgery include anaesthetic side effects, bladder problems, bleeding, device failure, dural tears, ileus, incision problems, infection, pain, paralysis, spinal fluid leakage, or death.
Usually, artificial disc replacement patients are discharged from the hospital about four days after surgery if there are no complications. Some physical limitations the patient has are no rotation of the lumbar region for three weeks after surgery, no curving of the lumbar region or intense stomach exercise for six weeks, no participation in sports for three months, no activities that stretch the sciatic nerve, and the need to ensure correct posture to avoid putting pressure on the prosthesis.
Artificial disc replacement is a safe and effective treatment for mechanical back pain caused by DDD. The success of an artificial disc replacement procedure depends on proper patient selection, diagnosis, and specialised surgeon experience with device placement. FDA data show that patients who have undergone artificial disc replacement experience results comparable to patients who have undergone spinal fusion. Only a select population of patients will be eligible for total disc replacement. It is predicted that approximately 20% of all patients with lower-level DDD will have artificial disc replacement surgery within two years.
Conclusion
Back pain is a common health problem for many people. One of the leading causes of back pain is Degenerative Disc Disease (DDD). Spinal fusion was the number one procedure for solving back pain for years because of DDD. Now, doctors are using artificial discs to replace diseased discs. The artificial disc offers an alternative to spinal fusion for treating degenerative disc disease at these levels. It is designed to preserve spinal motion and recreate the natural function of the disc. It is a safe and effective surgery for back pain caused by DDD.
References
- Strong, supple backs (1998) New Woman, 1 Apr. 1998: 38.
- Accucare Performs its 100th Successful Herniated Disc Procedure Using Breakthrough, Minimally Invasive Outpatient Technique: HydroDiscectomy. Business Wire, 3 April 2006
- Discectomy; Studies from S. Rasmussen and co-researchers in the area of discectomy published. Medical Devices & Surgical Technology Week, 19 Oct. 2008: p. 131.
- STRATTON, S. (2008) The Encyclopedia of the Back and Spine Systems and Disorders. p. 108-110.
- Alternative treatments to relieve back pain. Consumer Reports on Health, 1 Apr. 2006: 1,4-6.
- BAJNOCZY, S. (2005) Artificial disc replacement-Evolutionary treatment for degenerative disc disease. Association of Operating Room Nurses. AORN Journal, 82 (2), p. 192, 195-202, 205-6; quiz 207-12.
- Artificial Disc Replacement As Good Or Better Than Spinal Fusion Surgery. Targeted News Service, Washington, D.C. 26 Feb. 2009
- Irvine Family Health Center and Spinal Decompression (2006) Irvine, California.
- Medtronic (2007) CD Horizon Legacy. Google Images. Published June 13, 2007. Updated April 17, 2009.
- Rush University Medical Center. Chicago, Illinois. (2008) Artificial Lumbar Disc Replacement
Page Reference
If you quote information from this page in your work, then the reference for this page is:
- McDANIEL, L. et al. (2009) Back Pain [WWW] Available from: https://www.brianmac.co.uk/articles/article062.htm [Accessed
About the Authors
Larry W. McDaniel, Ed.D., is an Associate Professor of Exercise Science at Dakota State University, Madison, SD. USA. Dr McDaniel was a First Team All-American football player (USA Football), a Hall of Fame Athlete, and a Hall of Fame Wrestling Coach.
Allen Jackson, M. Ed., is an Assistant Professor of Physical Education and Health at Chadron State College in Chadron, Nebraska (USA), who is well known for his presentations and publications at international conferences focusing on Leadership, Curriculum, and Health.
Laura Gaudet, PhD., is a Professor and Chair of the Department of Counselling, Psychology and Social Work at Chadron State College, Chadron, NE.
Carmyn Streitz, Dakota State University, is an outstanding student of Exercise Science.