

Strength
Strength Training for Throwers
Davin Boydstun and Professor Allen Jackson suggest increasing strength for track athletes participating in the throwing events.
 Every collegiate-level track and field event requires high speed, strength, and coordination. Athletes in these events need as much of an explosive burst of speed and quickness as an athlete, combined with impeccable balance and extreme speed and strength (power). Strength is that rare attribute that can increase other skills as it is enhanced. Throwers may require any event's unique strength training regimen in track and field.
Every collegiate-level track and field event requires high speed, strength, and coordination. Athletes in these events need as much of an explosive burst of speed and quickness as an athlete, combined with impeccable balance and extreme speed and strength (power). Strength is that rare attribute that can increase other skills as it is enhanced. Throwers may require any event's unique strength training regimen in track and field.
There are a few crucial variables to focus on when developing these attributes:
- Closed-circuit resistance should be the heart of your resistance training.
- Every exercise should directly correlate to the event you are training for
- The core is the base for stability in everything you do.
Closed kinetic chain (or closed circuit) training is defined as an exercise where the "proximal extremity moves about a fixed distal extremity" (Moses 2009)[2]. Every throw in track and field is delivered from a position where the body's feet (the distal extremities) are fixed to the ground. In track and field, every throw is delivered from a position where the body's feet (the distal extremities) are fixed to the ground.
Although every throw involves "one-foot" or "no-feet" phases, the work is done when both feet are on the floor. Throwers must train their bodies to recruit and activate as many muscle fibres as possible from a closed-circuit position quickly and simultaneously. Thus, closed-circuit resistance becomes the focus of strength training.
 When correlating a weight training program to the throws, it is essential to match the lifts to similar muscle firing sequences, explosiveness, power, and angles of the throws. Olympic-type lifts should be a staple in a thrower's workout. These lifts start at the ground, working through the legs, incorporating hip thrust, tightening the core, engaging the upper trunk, and ending with all the energy produced exploding through the arms, creating a slight "whipping" motion. It has a very similar muscle firing sequence, minus the explosive extension of the arms, and can be done with a heavyweight. There are three basic Olympic lifts: power cleans, snatches, and jerks (including deadlift).
When correlating a weight training program to the throws, it is essential to match the lifts to similar muscle firing sequences, explosiveness, power, and angles of the throws. Olympic-type lifts should be a staple in a thrower's workout. These lifts start at the ground, working through the legs, incorporating hip thrust, tightening the core, engaging the upper trunk, and ending with all the energy produced exploding through the arms, creating a slight "whipping" motion. It has a very similar muscle firing sequence, minus the explosive extension of the arms, and can be done with a heavyweight. There are three basic Olympic lifts: power cleans, snatches, and jerks (including deadlift).
 |
 |
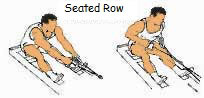 |
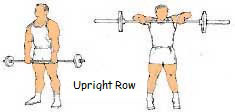
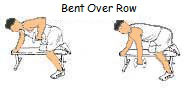
The development of the upper back is crucial to a thrower. These are the heavy lifts where throwers develop their power. These lifts will increase strength in the muscles that are used to throw. Again, throwers should use many variations of these lifts. Some examples are back squats, front squats, box squats, ¾ squats, squat jumps, sumo dead-lift, straight-leg dead-lift, elevated dead-lift, incline bench presses, decline bench presses, negative bench presses, bench press throws, one-arm rows, machine rows, etc. Again, using different angles will stimulate the development of the muscles.
 |
 |
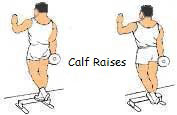 |
The focus of auxiliary lifts should be more muscle-specific and provide symmetry and balance in the body. The hamstrings, shoulders, and triceps are crucial to throwers; therefore, they should be the main focus. The calves and ankles provide the base and stability for a thrower and should be fully developed.
Given the torque throwers put on their midsections, core training is vital. Core training should focus on the external obliques, with a secondary focus on the latissimus dorsi, erector spinae, and rectus abdominis.
References
- JUDGE, L. (2008) Complete Track and Field Conditioning: Throws [Diagrams] USA: Coaches Choice
- MOSES, S. (2009) Strength Training [WWW] Available from:www.fpnotebook.com/Sports/Exercise/StrngthTrng.htm [Accessed August 2009]
Page Reference
If you quote information from this page in your work, then the reference for this page is:
- JACKSON, A. and BOYDSTUN, D. (2009) Strength Training For Throwers [WWW] Available from: https://www.brianmac.co.uk/articles/article050.htm [Accessed
About the Authors
Davin Boydstun is a Graduate Assistant working with the Chadron State College track team and coaching the CSC throwers. After graduation, Davin plans to continue his coaching career at the college level.
Allen Jackson is an Assistant professor in the Department of Health, Physical Education, and Recreation at Chadron State College.