

Injury Prevention
ACL Rehabilitation: Getting Back in the Game
Lyn Ausdemore, Chris Green, Tyler Lathrop, Zalie Limbach & Allen Jackson share thoughts on Anterior Cruciate Ligament rehabilitation.
Once an injury occurs, rehabilitation must take place to heal. Rehab can take weeks or months, depending on the severity of the injury. Many athletes do not take rehab exercises seriously and will not complete the whole rehab schedule. While many do the exercises, they do them incorrectly. One factor that causes many re-occurring injuries is poor technique during rehabilitative exercise. Many young athletes may never experience full recovery until they understand that improper technique is the cause of the ongoing problem. When you are in recovery, the information received can be beneficial and provide the analysis recovery based on performance and personal commitment. This paper focuses on injuries occurring to the Anterior Cruciate Ligament (ACL) and what it takes to overcome such adversity.
Cluett (2008b)[3] explained the function of the anterior cruciate ligament (ACL) as the primary resisting force to forward motion of the tibia. The anatomical construction of the knee joint helps in understanding this relationship (Cluett, 2008b)[3].
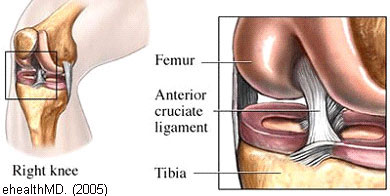
The femur (thigh bone) sits on top of the tibia (shin bone), and the knee joint allows movement at the junction of these bones. Without ligaments to stabilize the knee, the joint would be unstable and prone to dislocation. The ACL prevents the tibia from sliding too far forward. (Cluett, 2008b, p.1)[3] The ACL is a broad ligament joining the anterior tibial plateau to the posterior femoral intercondylar notch (Cross, 1998)[1].
The stabilization process of the ACL has four complex functions:
- It maintains mechanical stability
- restrains anterior translation of the tibia
- prevents hyperextension of the knee
- acts as a secondary stabilizer to valgus stress by reinforcing the medial collateral ligament and controlling the tibia's rotation on the femur in femoral extensions of 0-30 degrees. (Cross, p.1)[1]
ACL injuries are common problems involving the knee joint
Recent studies indicate that 1 in 10 female college athletes have sustained this type of injury sometime during their athletic carrier. Research suggests that females are participating in activities that "require cutting and jumping activities were five times more likely to suffer serious knee injuries compared to their male counterparts" (NWS, 2008, p.1)[7].
The ACL femoral attachment has a unique topography with a constant presence of the lateral intercondylar ridge and often a bony ridge between anterior medial (AM) and posterior-lateral (PL) femoral attachment to as the lateral bifurcate ridge. In the knee joint anatomy, an intercondylar notch lies between the lateral and medial condyles of the femur.
 The ACL is more vulnerable to some people than others. This is based on osseous landmarks of the femoral attachment of the ACL.
The ACL is more vulnerable to some people than others. This is based on osseous landmarks of the femoral attachment of the ACL.
The ACL femoral attachment has a unique topography with a constant presence of the lateral intercondylar ridge and often an osseous ridge between anterior medial (AM) and posterior-lateral (PL) femoral attachment; commonly referred to as the lateral bifurcate ridge. In the anatomy of the knee joint, an intercondylar notch lies between the lateral and medial condyles of the femur.
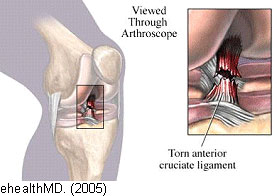
The ACL moves within this notch, connecting the femur and the tibia, thus stabilising the knee. The ACL prevents the tibia from sliding forward and rotating medially. The majority of females have a small notch, therefore restricting ACL movement. "When movement is restricted, the femoral condyles can pinch the ACL within the joint, especially during twisting or hyper-extended movements often resulting in a tear or rupture of the ligament" (Vlach, 2008)[11]. For some athletes, especially females, these attachment points may be smaller, contributing to female susceptibility to ACL injuries.
Assessment
An assessment must be done to know exactly what damage has occurred with all knee injuries. "The knee needs to be examined systematically since so much can go wrong with the knee, and so many signs and symptoms may be produced, that only a systematic technique will ensure that nothing of importance is missed" (Neyret et al. 2008, p. 1)[5].
Three different tests can be performed:
- the Lachman test
- the dynamic extension test
- the Pivot Jerk test (Cross, 1998)[1].
The most important out of these three tests, the Pivot Jerk test, was first described by M. Lemaire, in 1968.
- The patient's foot is wedged between the body and the elbow of the examiner
- The examiner places one hand flat under the patient's tibia, pushing it forwards (force applied in an anterior direction), with the knee in extension
- The other hand is placed against the patient's thigh, pushing the other way (force applied in a posterior direction)
- The lower limb is taken into slight abduction, by the examiner's elbow, with the examiner's body acting as a fulcrum to produce the valgus
- The examiner maintains the anterior tibial translation and the valgus and imparts flexion. At 20°-30° flexion, pivot shifting will occur, with a clunk as the lateral tibial plateau suddenly reduces. (Neyret et al. p.14)[5]
 |
 |
When this procedure produces a shift rather than a clunk, the patient is unaware of the slip of the plateaus on the femoral condyles. The valgus component is less pronounced than are the compression and anterior drawer applied by the examiner, therefore, producing joint play rather than a pivot shift, indicating a tear of the ACL.
Rehabilitation
There are many variations of ACL rehab that take considerable time to get back in proper physical condition. Each athlete has a specific rehab plan, even if many exercises are similar to another athlete. Each plan depends on a person's age, functional disability, and functional requirements (Cross, 1998)[1]. The major goals of rehabilitation following ACL surgery are:
- Restoration of joint anatomy
- Provision of static and dynamic stability
- Maintenance of the aerobic conditioning and psychological well being
- Early return to work and sport
Following ACL reconstruction surgery, the range of motion exercises starts immediately, with walking an essential component of post-operative rehabilitation. Being mobile during this time will help in incurring degrees involving the range of motion with the initial focus on regaining full extension of the knee. In general, flexion (ability to bend) is much easier to gain than extension (Cluett, 2008a)[2].
A typical rehabilitation program consists of four distinct phases. During the first phase, the emphasis is placed on minimizing pain, swelling, and maximizing motion. Throughout the second phase of rehab, increased ranges of motion are the main objective. During stage two, the patient is subjected to resistance training designed to increase the range of movement through a well-designed regiment of lifting exercises specific to the quadriceps and hamstrings.
The goal is muscle control, increased strength, and greater endurance during the third phase. At this stage, the range of motion should be completely back. During the final rehabilitation phase, the subject will be encouraged to gradually work back into their sport (Palmer, 2005b)[9].
Working with physical therapists is one way to make rehab more successful. Therapists know what and where someone should be during their specific program. They can make sure that one is not overdoing it. Overdoing it could result in not healing the injury properly. Different exercises that one can do tolerably include heel slide, isometric contraction of quads, and prone knee flexion. Other exercises that can be done once able to stand include passive knee extension, heel raise, half squat, knee extension, and standing on one leg. (Quinn, 2006)[10]
Getting patients on a stationary bike is a good way to regain motion and improve strength. Other activities that one can do are, working in a pool, on a trampoline, wobble board, and jogging, among many others. These activities are used during the different phases, so do not think one can be on a wobble board right after surgery. Take things slow and make sure that the injury heals correctly so that one does not end up back at the beginning of rehab.
Once rehab is finished, the doctor will have an ultimate say in returning to a sport or working fully.The doctor's decision can be based on how well one did during rehab and the graft type (if one was done). Specific grafts are believed to take longer to heal, and therefore, the doctor may not want to push the knee too far too soon. The athlete may ask the question of "should I wear a brace?" It all depends on the athlete. Some prefer a brace, while others do not. No studies show that a brace helps or harms one when wearing it (Cluett, 2008a)[2]
Palmer (2005a)[8] offers some encouraging information for all to consider: Many struggle to regain form after a serious sports injury and lengthy rehab period, some take months or fail. Getting back into form will be slow if we do not know exactly what i needs to be recovered. A natural talent for a sport comes from the right sort of conditioning. Good quality movement executed in the sporting activity sets up appropriate learned movement patterns that reside subconsciously. (Palmer, 2005a, p. 2)[8]
Conclusion
Rehabilitation is defined in NRI (2008)[6] as a combination of methods focusing on restoring a subject's useful life. Regardless of the disabling experience, rehabilitation helps the body achieve normal functions through different recovery techniques. Suppose a person has experienced a sports injury, an accident, or is incapacitated due to other reasons. In that case, rehabilitation can improve the functionality of movements and also help in maximizing personal health characteristics. Through rehabilitation, "not only is the physical aspects covered, but also the mental, psychological and sociological aspects in achieving full recovery." (NRI, 2008, p. 1)[6]
Rehabilitation from injuries requires constant care by providing exercise therapies to regain muscles lost and recover from trauma experienced by allowing contact to other patients who have experienced similar injuries. Injuries involving young athletes' original skill patterns are often replaced by newly acquired poor-quality action following a sports injury. Some athletes never regain the ability to realize their full potential after an injury requiring rehabilitation. (Palmer, 2005a)[8]
References
- CROSS, M.J. (1998) Anterior Cruciate Ligament Injuries: Treatment and Rehabilitation. Encyclopedia of Sports Medicine and Science
- CLUETT, J. (2008a) Rehabilitation After ACL Surgery. About.com: Orthopedics
- CLUETT, J. (2008b) ACL injury. About.com: Orthopedics
- ehealthMD. (2008) What is the anterior cruciate ligament? Health Information Publications
- NEYRET, P. et al. (2008) Examination of the knee joint
- NRI, (2008) Importance of rehabilitation. NewRehabilitationInfo.com
- NWS, (2008) Female ACL. New Wave Soccer Conditioning
- PALMER, R. (2005a) Rehabilitation: Time to Assess. Fitness Programs for Life
- PALMER, R. (2005b) Sports Injury Rehabilitation: Learn to take it Easy! Fitness Programs for Life
- QUINN, E. (2006) ACL Rehab Exercises. About.com: Sports Medicine
- VLACH, S. (2008 ACL and the female athlete: Theoretical causes and prevention. Life Fitness
Page Reference
If you quote information from this page in your work, then the reference for this page is:
- JACKSON, A. et al. (2009) ACL Rehabilitation: Getting Back in the Game [WWW] Available from: https://www.brianmac.co.uk/articles/article048.htm [Accessed
About the Authors
Lyn Ausdemore, Tyler Lathrop, & Zalie Limbach are all upper-division students seeking degrees with endorsements in human performance. Chris Green is a trainer for the athletic department, and Allen Jackson is an Assistant Professor for the Department of Health, Physical Education and Recreation at Chadron State College.